Background Despite extensive data examining perioperative risk in patients with coronary artery disease, little attention has been devoted to the implications of conduction system abnormalities.
Objective To define the clinical significance of bundle-branch block (BBB) as a perioperative risk factor.
Bạn đang xem: Bundle-Branch Block as a Risk Factor in Noncardiac Surgery
Methods Retrospective, cohort-controlled study of all noncardiac, nonophthalmologic, adult patients with BBB seen in our preoperative evaluation center. Medical charts were reviewed for data regarding cardiovascular disease, surgical procedure, type of anesthesia, intravascular monitoring, and perioperative complications.
Results Bundle-branch block was present in 455 patients. Right BBB (RBBB) was more common than left BBB (LBBB) (73.8% vs 26.2%). Three patients with LBBB and 1 patient with RBBB died; 1 patient had a supraventricular tachyarrhythmia. Three of the 4 deaths were sepsis related. There were 2 (0.4%) deaths in the control group. There was no difference in mortality between BBB and control groups (P=.32). Subgroup analysis suggested an increased risk for death in patients with LBBB vs controls (P=.06; odds ratio, 6.0; 95% confidence interval, 1.2-100.0) and vs RBBB (P=.06; odds ratio, 8.7; 95% confidence interval, 1.2-100.0).
Conclusions The presence of BBB is not associated with a high incidence of postoperative cardiac complications. Perioperative mortality is not increased in patients with RBBB and not directly attributable to cardiac complications in patients with LBBB. These data suggest that the presence of BBB does not significantly increase the likelihood of cardiac complications following surgery, but that patients with LBBB may not tolerate the stress of perioperative noncardiac complications.
RECENT CHANGES in the practice of anesthesiology have resulted in anesthesiologists assuming a larger role in perioperative care. Accurate preoperative risk assessment is an important component of these expanded responsibilities. Unfortunately, there are insufficient data regarding perioperative implications for many commonly encountered medical conditions. Included in this category are abnormalities of the cardiac conduction system distal to the atrioventricular node, commonly referred to as bundle-branch disease. This electrocardiographic (ECG) abnormality is a common finding in the elderly general medical population, who represent an increasing percentage of patients undergoing elective surgery. Data from the Framingham Study indicate that the appearance of bundle-branch block (BBB) is almost always clinically silent, but is often associated with the presence of cardiovascular abnormalities.1-3 The Framingham Study also demonstrates that patients with newly acquired BBB had an increased likelihood of development of coronary artery disease and congestive heart failure, and a 3- to 4-fold higher mortality rate. The presence of BBB can also interfere with ECG detection of myocardial ischemia4 and assessment of previous myocardial infarction.5
The loss of diagnostic accuracy and the increased likelihood of cardiovascular disease in patients with BBB may explain the common practice of performing extensive testing in this population. These costly preoperative workups are only justified if perioperative risk is significantly increased in this population. Unfortunately, available data do not adequately define the risk. Goldman et al6 noted a 5% incidence of cardiac death in patients with intraventricular conduction abnormalities. Although multivariate analysis did not indicate BBB to be an independent predictor of cardiac death, this may reflect the small sample size in the study by Goldman et al. Berg and Kotler7 also noted a high mortality rate in surgical patients with BBB (10%), but only 30 patients with BBB underwent evaluation. Thus, there remains considerable uncertainty regarding the preoperative significance of BBB. Given the paucity of data in the literature examining perioperative risk in patients with BBB, we undertook a retrospective chart review of all patients with BBB undergoing elective surgery who entered the hospital through the preoperative evaluation center (PEC) of The Johns Hopkins Hospital, Baltimore, Md. We then randomly selected a group without BBB but with similar age, sex, American Society of Anesthesiologists (ASA) classification, and type of surgery. Our objective was to determine the mortality and risk for intraoperative and/or postoperative cardiovascular complications in patients with BBB and to compare their mortality with that of a control population.
Standard practice in our PEC during the study period was to obtain preoperative ECGs on all patients older than 40 years and on younger patients with significant clinical risk factors for heart disease (diabetes mellitus, hypertension, or strong family history or symptoms of coronary artery disease or heart failure). History numbers of all patients seen in the PEC from January 1, 1991, through December 31, 1995, with BBB were obtained by querying the Department of Cardiology Heart Station computer (MUSE System, Marquette Electronics, Milwaukee, Wis) for cardiologist-interpreted ECGs with right BBB (RBBB) or left BBB (LBBB). We prospectively excluded children (aged <18 years) and adult patients undergoing cardiac or ophthalmologic procedures. Patients undergoing outpatient cardiac surgery were excluded because, during the study, they represented a small, atypical number of total patients undergoing cardiac surgery. Patients scheduled for ophthalmologic procedures were not evaluated in the PEC and were excluded because of the minimal invasiveness of their surgical procedure.
Xem thêm : White Spots on My Baby’s Teeth: What is it?
Medical records for patients with BBB were examined to confirm the presence of BBB at the time of the surgical procedure. We classified BBB as new if it was not present on a previous ECG or if there was no previous ECG available (this definition was used because this is the situation encountered by clinicians when they are evaluating BBB). Demographic data, including age, sex, ASA classification, type of surgical procedure, presence of known cardiovascular abnormalities, cardiovascular medications, type of anesthesia, and use of intraoperative invasive monitoring devices, were recorded, and the hospital course was reviewed to determine if death or cardiovascular complications occurred (death, myocardial infarction, unstable angina, pulmonary edema, or arrhythmia).
The control group was composed of randomly selected patients without BBB who were seen in the PEC from January 1, 1994, through December 31, 1995, and who were undergoing nonophthalmologic, noncardiac surgery. This group was matched on the basis of postsurgical disposition (ambulatory and same-day admission). Demographic data (age, sex, ASA classification, and type of surgery) were compiled, and the hospital case-mix database was used to detect in-hospital mortality.
We estimated that 461 patients would be needed in each group to provide the study with a power of 80% to detect an increase in mortality from 0.4% (cohort group) to 3.0% (BBB group) at the .05 level. We used 3.0% mortality based on previously published work by Goldman et al6 that showed a 5% incidence of cardiac death in patients with intraventricular conduction abnormalities. We assumed that a 40% improvement in event rate had occurred since the publication of this data in 1978.
We used χ2 and t tests to compare demographic data and anesthetic technique in patients with LBBB and RBBB. The χ2 test was also used to compare the incidence of new patients with LBBB or RBBB. Two-tailed Fisher exact test was used to compare mortality and complications in patients with LBBB and RBBB, in patients with new and established BBB, and in patients with and without BBB. Pearson product moment correlation was used to evaluate the impact of age and sex on death. Significance was determined at P<.05.
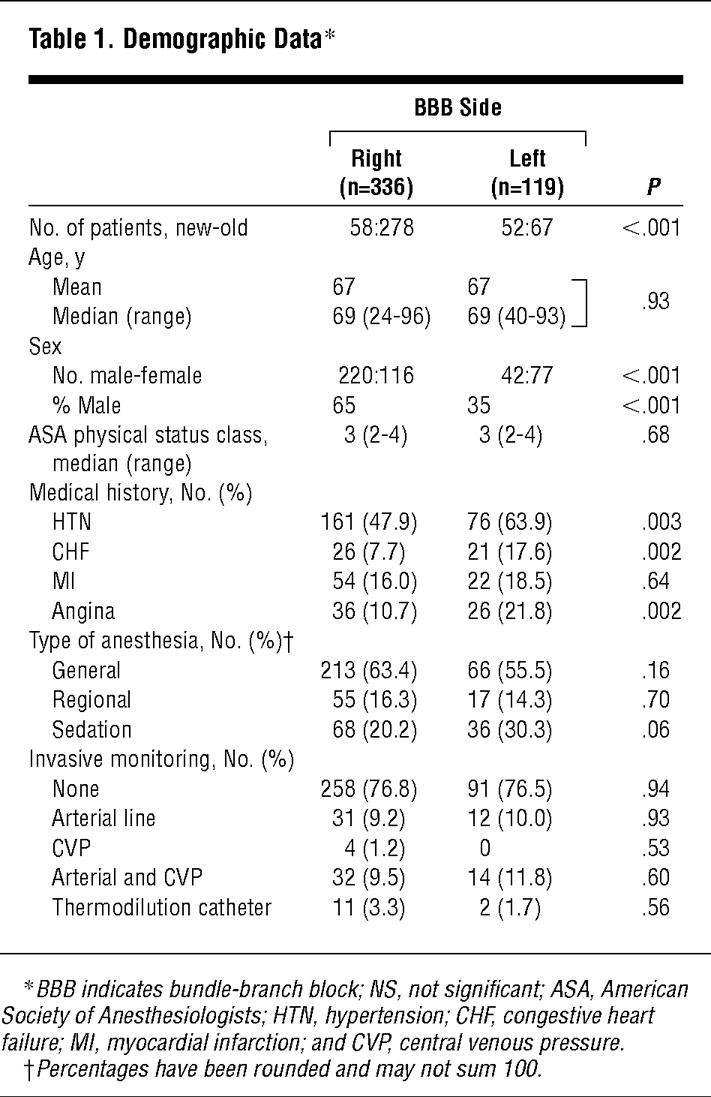
The PEC examined 25 539 adult patients during the study. The MUSE System identified 535 (2.1%) patient history numbers that met BBB criteria. Twenty patients underwent more than 1 procedure, but were considered only once (these 20 patients sustained no complications). Forty patients scheduled for cardiac surgery and 20 children were excluded. The remaining 455 patients consisted of 119 patients with LBBB (26.2%) and 336 with RBBB (73.8%) (Table 1). Bundle-branch block was considered new in 52 (43.7%) of 119 patients with LBBB and in 58 (17.3%) of 336 patients with RBBB (P<.001, LBBB vs RBBB). Right BBB was more common in men, whereas LBBB was more common in women.
More than half of the patients with BBB had hypertension, and 10.3% had a history of congestive heart failure; both conditions were more common in patients exhibiting LBBB. Angina was present in 13.6% of patients with BBB and was more frequent in patients with LBBB. History of myocardial infarction was seen in 16.7% of patients with BBB, and the incidence was similar for LBBB and RBBB. Preoperative medication use was not different between groups, except patients with LBBB had increased diuretic use (P=.005). Intraoperative invasive monitoring (arterial, central venous, or thermodilution catheters) was used in 23.3% of patients with BBB, which was not different between RBBB and LBBB groups, and intraoperative anesthetic management was not different between BBB groups.
There were 460 patients in the randomly selected non-BBB control cohort. Median ASA physical status was 3 (range, 2-4) in both BBB groups and in the control group. Patients with BBB and controls underwent similar surgical procedures in most circumstances (Table 2). In the BBB and control groups, 22.0% and 21.7% of patients, respectively, underwent ambulatory procedures, whereas the other 78.1% of all patients were admitted after surgery. Although the patients with BBB were slightly older and more commonly male compared with controls (Table 2), these differences were not associated with mortality (P=.90 and P=.98, respectively).
No cardiovascular complications were observed in the patients with BBB intraoperatively. Postoperatively, no patients with BBB experienced myocardial infarction, pulmonary edema, or ventricular dysrhythmias. Atrial fibrillation developed in 1 patient with LBBB. Four patients with BBB (0.9%) died postoperatively (Figure 1), due to stroke after repair of an arteriovenous malformation (n=1; RBBB group) and sepsis (n=3; LBBB group). Two of the sepsis-related deaths occurred after prolonged hospitalizations (>30 days), one of these after a left inguinal hernia repair, and another after supraglottic resection of squamous cell cancer. The third patient with sepsis died on postoperative day 4 following a radical cystectomy for bladder cancer. All 3 patients in the LBBB group with deaths due to sepsis had known heart disease; 2 of these had heart failure and 1 had a previous myocardial infarction and reduced ejection fraction. The patient in the RBBB group had a history of hypertension. There were 2 (0.4%) deaths in the control cohort. The first occurred after removal of cervical spine hardware and the second was due to sepsis after a sigmoid colectomy.
Xem thêm : Fast Pace Urgent Care to Partner With Calcasieu Urgent Care
There are 2 major findings of this study. First, the study confirms that cardiovascular disorders are common in patients with BBB presenting for elective surgery.1-3 Second, perioperative cardiovascular complications are uncommon in patients with BBB. Although the mortality rate is low in patients with RBBB, it remains unclear whether patients with LBBB may be at a higher risk for postoperative morbidity and mortality secondary to poor myocardial reserve that is clinically represented by an intolerance to certain stress states such as severe sepsis.
Chronic BBB is present in about 1% of the adult US population,8 but there is very little known about the perioperative implications. The Framingham Study, the largest prospective study of acquired BBB, did not specifically address the perioperative period.1-3 Bundle-branch block developed in approximately 2.3% of patients in the Framingham Study during the 16-year period they were observed. This is similar to the 2.1% incidence of BBB in our patients presenting for surgery. In the Framingham Study, the prevalence of RBBB was greater in men, a finding supported by our study. The Framingham Study also demonstrated that the appearance of BBB is frequently clinically silent and that individuals with acquired BBB are more likely to have preexisting hypertension (60%), coronary artery disease (10%), and congestive heart failure (4%). Moreover, coronary artery disease and congestive heart failure were more likely to develop in individuals with acquired BBB over time (20%-30% incidence of each); they had a cumulative cardiovascular disease mortality rate of 3 to 4 times greater than the general population. Men with RBBB did not demonstrate an increased likelihood of cardiovascular abnormality by multivariate analysis, whereas women with LBBB or RBBB were more likely to have cardiovascular disease. There was also a trend toward a higher mortality rate in individuals with LBBB as opposed to RBBB. Studies in hospitalized patients and community-based and military populations have also suggested that RBBB is more likely to occur in persons of both sexes without cardiovascular disease than is LBBB.8-12 As a result, many clinicians consider LBBB to be a marker of cardiovascular dysfunction. As a corollary of this assumption, patients with LBBB are often thought to be at increased risk for perioperative cardiac complications.
Goldman et al6 observed a 5% incidence of cardiac death in patients with intraventricular conduction abnormalities, but BBB was not an independent predictor of death (small sample size). The only other published study, by Berg and Kotler7 in 1971, examined 30 patients with bilateral BBB (RBBB with left axis deviation or LBBB with first-degree heart block). There were no intraoperative deaths and no episodes of intraoperative complete heart block. However, 3 (10%) of their patients died postoperatively, 1 patient due to a myocardial infarction.
The observed low incidence of perioperative cardiac morbidity and mortality in our patients with BBB suggests that BBB alone is not an independent risk factor for cardiac complications. Although the finding of BBB should alert the perioperative physician to the possibility of occult coronary artery disease or impaired left ventricular function, our data suggest that patients with BBB who do not have overt signs or symptoms of coronary artery disease or congestive heart failure do not require extensive preoperative cardiac evaluation. This is consistent with the Framingham data and those of other studies, which demonstrate that mortality risk increases with the presence of cardiovascular disorders.
Our study has certain limitations that the reader must consider when interpreting our findings. First, our surveillance was chart based, and, therefore, may have underestimated the incidence of perioperative cardiac events, because only clinically apparent (not subclinical) complications were noted. We are confident of the mortality data from chart review and the hospital case-mix database, which have been well evaluated.13 Second, our study lacks sufficient power to detect a small increase in mortality (<1.6%) in patients with BBB. To detect this difference would require many more patients and a multicenter trial. Third, our study lacks sufficient power to detect a difference between LBBB or RBBB and controls. Consequently, we believe that the conservative interpretation of the trend toward an association between LBBB and late death due to sepsis is that patients with LBBB may not tolerate the increased stress of noncardiac complications. This would be consistent with previous studies demonstrating that patients with sepsis and cardiovascular dysfunction have increased mortality.14 Fourth, our study was performed on patients presenting for elective surgery, and it should not be assumed that these data can be extrapolated to hospitalized patients or those undergoing emergency surgery.
We have demonstrated that preoperative BBB is associated with significant abnormalities of the cardiovascular system, but does not appear to be a major risk factor for the development of perioperative cardiac complications. Left BBB, but not RBBB, may be associated with increased postoperative mortality, although not directly attributable to cardiovascular complications. Further study is necessary to evaluate prospectively cardiovascular complications and mortality in a larger cohort of patients with BBB.
Accepted for publication June 29, 1999.
Reprints not available from the authors.
Corresponding author: Todd Dorman, MD, The Johns Hopkins Hospital, Department of Anesthesiology, 600 N Wolfe St, Meyer 299A, Baltimore, MD 21287-7294 (e-mail: tdorman@jhmi.edu).
Nguồn: https://blogtinhoc.edu.vn
Danh mục: Info
This post was last modified on Tháng mười một 22, 2024 3:21 chiều