Cornea: Device focusJuly 2016
by Michelle Dalton EyeWorld Contributing Writer
Cornea experts caution about using the tissue as a cure-all for every corneal disorder
Amniotic membrane (AM) is designed for use with specific corneal and conjunctival diseases, with proposed uses including persistent epithelial defect, prevention of ocular complications associated with Stevens-Johnson syndrome, primary/recurrent pterygia, cicatricial pemphigoid, and conjunctival forniceal reconstruction. AM assists in wound healing and prevents scar tissue formation as it has powerful antifibrotic and anti-scarring properties.
Bạn đang xem: Blog
But what it is not, experts say, is a substitute for a bandage contact lens.
“For disadherence problems, AM is not the solution because it doesn’t address the disadherence. It only gets surface defects to heal, but there will still be problems with adherence,” said John Hovanesian, MD, clinical instructor, Jules Stein Eye Institute, Los Angeles, adding something like a neurotrophic cornea would be an appropriate use of AM.
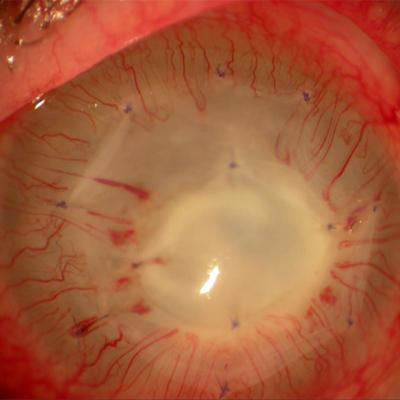
Persistent corneal defects are the most common use of AM for Anthony Aldave, MD, professor of ophthalmology and chief of the cornea and uveitis division, Jules Stein Eye Institute. “Other uses that are less common include the management of painful, bullous keratopathy in eyes with poor visual potential,” Dr. Aldave said.
There are 2 types of commercially available AM—cryopreserved and dehydrated. The cryopreserved version (PROKERA, Bio-Tissue, Doral, Florida) includes a solid plastic ring that encompasses the cornea and sits on the conjunctiva; AmnioGraft (Bio-Tissue) does not. The dehydrated form (AmbioDisk, IOP Ophthalmics, Costa Mesa, California) is a sutureless overlay AM disk. PROKERA is available in 3 versions (slim, traditional, and plus), and the dehydrated form also includes Ambio2 and Ambio5, with various thicknesses and diameters.
In the last 30 years there has been no reported case of bio-incompatibility, rejection, or allergic reaction to AM, said Neel Desai, MD, partner, the Eye Institute of West Florida, Largo, Florida. “Both types of AM are very safe.”
Differences between types of AM
There are “very clear differences in the function and the cellular architecture and the biological activity between cryopreserved membrane and dehydrated membrane,” Dr. Desai said. For the dehydrated membrane to be self-retaining, it has to use a contact lens in conjunction. The PROKERAs design means it is self-retaining.
The cryopreserved versions need to be stored in a freezer for prolonged storage, whereas the dehydrated version is “shelf stable,” and typically has a long shelf life, Dr. Hovanesian said.
Drs. Hovanesian and Desai said both types of AM work well, but for potentially different scenarios. Dr. Desai uses cryopreserved AM when patients have “excellent vision potential and I need to ensure the defect or corneal dystrophy is resolved quickly and without scarring with 1 single intervention.” When he’s more concerned with providing some extracellular matrix with the membrane and the vision potential is limited, then he will consider the dehydrated form.
“The biological activity of the cryopreserved tissue means I get faster healing more consistently with less scarring and haze than I do with the dehydrated versions,” Dr. Desai said. “In eyes that I’m not trying to improve for refractive cataract surgery, a dehydrated membrane is great because it provides wound coverage, and it gets the cornea healed eventually.”
Xem thêm : Tim Hortons: Caffeine Per Dollar
Dr. Hovanesian indicated that in extensive use of both types of amniotic membrane, he has not seen a difference in biologic activity, and assays of dehydrated AM have shown the presence of biologically active components similar to cryopreserved tissue. Furthermore, because the dehydrated form comes in various thicknesses, it can be used for conjunctival reconstruction or to form a new conjunctiva where a thicker membrane is advantageous, Dr. Hovanesian said.
Dr. Desai uses the dehydrated forms in cases of neurotrophic ulcers that are already scarred or in infectious keratitis.
“In many cases, though, I may need to reapply a dehydrated membrane twice or 3 times before the cornea is fully healed,” he said. He also advised against using PROKERA in patients with previous filtering surgery “where the PROKERA ring would rub against that bleb and cause potential problems.”
Misperceptions
AM is sometimes perceived as useful only in “train wreck” situations, but “we don’t want to wait until there’s already a scarring process or inflammatory process underway before we utilize this technology,” Dr. Desai said.
But that doesn’t mean its use is appropriate in all cases, Dr. Hovanesian added.
“This is not a cure-all to be used for every possible cornea problem,” Dr. Desai said.
Too often, AM is used for indications for which it is not well suited, which, in turn, delays a more definitive and appropriate treatment, Dr. Aldave said. He cited cases of patients who had AM placed for significant corneal stromal thinning; in cases in which the AM does not stop the progression of thinning, the cornea may perforate, necessitating the placement of cyanoacrylate glue, “which is more difficult to perform after as opposed to before corneal perforation.”
Dr. Hovanesian thinks the biggest misperception about when to use AM is in cases of dry eye or epithelial basement membrane dystrophy or “anytime you’ve got an ocular surface disease.”
“It’s not wrong to use AM in dry eye, but it’s a very rare case of dry eye that actually needs AM,” he said. Using AM in just any dry eye patient “is not generally helpful.”
Inflammatory processes are in play with ocular surface disease (OSD), making it a chronic condition with acute flare-ups. But “the number of instances where you might want to resolve an acute upon chronic flare-up with an AM are going to be few and far between,” Dr. Desai said. “We don’t want to treat with AM before the patients been on topical steroids and topical cyclosporine 0.05% and before we’ve tried some of the newer topical therapies for OSD.”
Dr. Aldave has been referred cases where AM was used in the treatment of a persistent epithelial defect overlying active infectious keratitis or scleritis. In neither case is AM an appropriate treatment as it does not possess antimicrobial properties and obscures the underlying infectious process.
Dr. Hovanesian has seen referral patients with AM for recurrent erosions—a sometimes inappropriate treatment. Using AM as a bandage for basement membrane dystrophy is reasonable, “but I don’t think it has any significant advantage over a collagen bandage contact lens, which is a much more cost effective way to address that issue.”
Xem thêm : Osteoporosis
Clinicians may think that using AM in the management of corneal limbal stem cell deficiency is appropriate, but “applying AM is not going to address the underlying problem as it is not a source of limbal stem cells,” Dr. Aldave said.
While no one thinks clinicians are intentionally misusing AM, “it comes down to misunderstanding what AM can and cannot do based on not being familiar with its biologic properties,” Dr. Aldave said.
Pearls for use
“Don’t wait to treat when there’s a good indication to do it and prevent vision loss by using AM, but be cautious about overusing it in conditions that have a very loose indication,” Dr. Desai said.
Clinicians should note that the more inflammation there is, the faster the membrane is going to dissolve and release its biological factors.
“With PROKERA, the membrane may dissolve after 2 to 3 days, particularly in a hot eye,” Dr. Desai said. But since the removal of a global period of 10 days, if the patient will benefit from a second membrane, the surgeon can insert one “even at day 2 or 3.”
When AM is sutured to the cornea for management of persistent corneal epithelial defects, as it is very thin, it may not remain intact for the requisite period of time unless its protected. Therefore, Dr. Aldave said, “I always place a bandage contact lens and perform a suture lateral tarsorrhaphy to help maintain the contact lens. At 1 month after surgery, I open the tarsorrhaphy, take out the contact lens, and typically the epithelial defect has healed.”
Get patients invested in the process, Dr. Desai said.
“So much of what we do is absolutely painless that patients have this preconceived notion that everything should be painless,” he said. “We need to make sure that patients understand that it may be in their best interest to be a little bit uncomfortable for a day or 2 to give them the long-term best outcome with less scarring, less haze, better vision, faster healing, and fewer adverse events, like fungal keratitis, compared to just using a contact lens.”
When used properly, AM has amazing abilities, Dr. Hovanesian said.
“AM and the whole biologics industry is a powerful tool in our armamentarium as cornea specialists and eyecare professionals that treat any variety of ocular surface diseases,” Dr. Desai said.
Editors’ note
Dr. Aldave has no financial interests related to his comments. Dr. Desai has financial interests with Bio-Tissue. Dr. Hovanesian has financial interests with Katena (Denville, New Jersey).
Contact information
Aldave: aldave@jsei.ucla.eduDesai: desaivision@hotmail.comHovanesian: jhovanesian@harvardeye.com
Nguồn: https://blogtinhoc.edu.vn
Danh mục: Info
This post was last modified on Tháng mười một 21, 2024 4:37 chiều