Abstract
Injection drug use-associated infective endocarditis (IDU-IE) is a preventable infection with substantial morbidity and mortality. There is significant interest in quantifying the epidemiology, microbiology, economics, and clinical outcomes of IDU-IE to identify comprehensive evidence-based treatments and opportunities for practice improvement [1]. However, IDU-IE remains challenging to study given difficulties in assembling representative study cohorts and the propensity for persons who inject drugs (PWID) to seek care at multiple health care locations during the course of a single illness. Administrative data can provide a unified source of information for epidemiological studies given systematic collection of data over time. Several recent studies have sought to leverage these unique strengths to better understand IDU-IE [2-4].
Administrative data are constrained by the data set used (ie, who/what are included), the reason for its creation (they are often not created for the research in question), and the accuracy of the coding [5]. Many studies using administrative data never validate assumptions when building their cohort. Specifically, many studies do not include validation analyses on the diagnostic or procedural codes used [6]. Biases are often introduced based on the surrogates chosen for the diagnosis in question. For example, there is no specific ICD-10 diagnosis code for IDU-IE. Prior work using administrative data to evaluate outcomes for IDU-IE rely on combinations of ICD codes for both endocarditis and opioid use disorders [3, 4, 7-9]. However, these codes include nonspecific conditions. Commonly used ICD-10 codes in endocarditis studies include “rheumatic heart disease” and “other valvular disorders.” The most common opioid use disorder code is also frequently applied to patients receiving prescription opioids from their physician for chronic pain. We hypothesized that the combined use of nonspecific ICD-10 codes likely overestimates the national prevalence of IDU-IE and underestimates the emergence of co-occurring infectious diseases such as hepatitis B virus infection, all-cause mortality, and the use and benefit of medications for opioid use disorder (MOUD), including buprenorphine and methadone.
The aim of this study was to evaluate the accuracy of the most commonly used ICD-10 code combinations for identifying IDU-IE in administrative data sets. This included a validation study of existing ICD-10 codes to identify IDU-IE and an evaluation of the impact of misclassification on OUD outcomes reported in prior IDU-IE administrative data research.
METHODS
Data Source and Study Design
We compared a prospectively identified cohort of PWID with IDU-IE secondary to injection opioid use with a retrospective cohort identified using nonspecific ICD codes from prior published studies [4]. Both cohorts were comprised of patients treated at Barnes-Jewish Hospital, a 1400-bed academic medical center located in St. Louis, Missouri, between July 1, 2017, and May 1, 2020. We considered the prospective cohort the “gold standard” for the validation study.
Case Selection and Definitions
Patients in the prospective cohort were identified by infectious diseases physicians during routine patient care as part of a quality improvement initiative and later a CDC Developing Healthcare Safety Research contract [10]. The case form specifies the type of invasive infection and the type of substance used; only patients who had injection opioid use-associated endocarditis were included in this analysis. Cases were manually reviewed by an infectious diseases (ID) physician (L.R.M.) to verify that they met inclusion criteria (current injection drug use contributing to current episode of infective endocarditis). A second physician (L.J.) reviewed 50% of the charts at random to assess for data concordance. Only individuals with evidence of endocarditis on prospective chart review were considered IDU-IE cases.
Patients in the retrospective cohort were identified for screening from admissions during the same time frame as the prospective cohort, through use of the ICD-10 codes listed in Supplementary Table 1. For inclusion in the retrospective cohort, patients must have had both ICD-10 code F11.xx and at least 1 of the following ICD-10 codes related to endocarditis documented: I38, I33.0, I33.9, I35.8, B37.6, T82.6, I05.9, I01.1, I08.0, I08.3, I08.9, I37.8, I07.9, A38.2.
To assess the validity of ICD-10 diagnosis codes for identifying IDU-IE admissions, patient charts were individually reviewed by an infectious diseases (ID) physician (M.J.D., L.R.M., N.S.N.) to evaluate (1) if the hospital admission was related to infective endocarditis, (2) what clinical problem prompted the documentation of the code F11, and (3) if the patient’s infective endocarditis was presumed secondary to injection drug use. Using an iterative process, all reviewers (L.R.M., M.J.D., and N.S.N.) reviewed 10% of the charts at random to assess for data concordance. This process was repeated until concordance was >90%.
Patient Characteristics
Patient comorbidities were identified using elements from the Elixhauser comorbidity index [11]. Patient demographics, clinical covariates, 90-day readmission rates, against medical advice (AMA) discharge, and outcomes data were collected. Receipt of MOUD, comprised of buprenorphine, methadone, or either oral or intramuscular naltrexone, was assessed by review of medication administration records. Hepatitis B virus antigen, hepatitis C virus antibody, and causative pathogen were assessed by review of microbiology data from the electronic medical record (EMR). Mortality was assessed using both the EMR and the National Social Security Death Index. Patients were censored at either 1 year of postdischarge follow-up or May 1, 2020. We defined rural and urban location using patient zip codes for location data and Federal Office of Management and Budget definitions, categorizing all micropolitan and noncore counties as “rural” and all metropolitan counties as “urban” [12, 13].
Statistical Analyses
Performance of the ICD-10 codes for identifying IDU-IE admissions as determined by physician chart review was compared with the prospectively collected cohort. Chi-square and Fisher exact tests were used to compare categorical variables. Pooled 2-sample t tests were used to compare continuous variables. Sensitivity for IDU-IE was calculated for ICD-10 hospital discharge data, accepting physician review as a “reference standard.” Relative risk ratios (RRs) with 95% confidence intervals were calculated to determine the predictors of AMA discharge. Kaplan-Meier estimates were used to describe the survival distribution for time to readmission. The log-rank statistic was used to test the difference in time to readmission. Descriptive statistics were calculated using SPSS, version 26 (Armonk, NY, USA). Figures were created using GraphPad Prism 9 (San Diego, CA, USA). This study was approved by the Washington University Institutional Review Board.
RESULTS
Utility of ICD-10 Codes for Identification of IDU-IE
Xem thêm : Urinary Tract Infection (UTI) in Males
Few studies have validated ICD code algorithms for IDU-IE. A recent systematic review of the validity of ICD codes in identifying medical complications of illicit drug use found that no 2 studies have validated the same algorithm despite similar target conditions [14]. An ICD-10 code algorithm comprised of code F11.xx plus at least 1 endocarditis-related code (Supplementary Table 1) identified a total of 188 patients over the study period. However, ID physician review demonstrated that only 82 (43.6%) of these patients met clinical criteria for IDU-IE. Furthermore, the ICD-10 algorithm failed to identify an additional 44 patients identified on prospective review.
Prospective identification of IDU-IE over this time period yielded 114 patients. Of these, only 73 (64.0%) were also identified through electronic query using a combination of an endocarditis-related ICD-10 code (listed in Supplementary Table 1) and ICD-10 code F11. Patients identified by prospective review but not ICD-10 codes were frequently noted to be missing an ICD code for their underlying substance use disorder, despite physician documentation that endocarditis was related to underlying injection drug use. In some instances, the patient was noted to have multiple infections (eg, Staphylococcus aureus bacteremia complicated by endocarditis, septic arthritis, osteomyelitis, septic emboli, and endocarditis) with only some complications receiving an ICD-10 diagnosis code along with a diagnosis of septic shock. Chronic pain with prescription opioids was a commonly used ICD-10 diagnosis code that led to erroneous identification of IDU. Underling valvular disease was the most common ICD-10 diagnosis code that led to erroneous identification of IE. An additional 9 patients were identified by ICD-10 code combined with chart review, who were not identified by prospective physician review. All patients identified by prospective physician review and the additional 9 patients identified by ICD-10 code combined with chart review were included as confirmed IDU-IE cases (total 123 cases) in our subsequent analysis. The sensitivity of ICD-10 code combinations for identification of IDU-IE cases was 65%.
Analyses of patient demographics between the confirmed IDU-IE cases and noncases showed a statistically significant difference in age, length of stay, and multiple chronic comorbidities (Table 1). Overall, patients with IDU-IE were younger (mean age, 34 years; compared with 54 years for noncases). The median length of stay for IDU-IE was 40 days vs 5 days for non-IDU-IE cases. Patients with IDU-IE were more likely to lack stable housing (28% vs 7%; P = .001) and had higher rates of AMA discharge (15% vs 4%; P = .005). In addition to being older and more stably housed, non-IDU-IE cases had significantly higher rates of diabetes, congestive heart failure, malignancy, neurologic disorders, and depression.
Microbiologic characteristics significantly differed between the 2 groups, with IDU-IE cases more likely to be attributed to methicillin-susceptible Staphylococcus aureus, methicillin-resistant Staphylococcus aureus, or streptococcal species (Table 1). While S. aureus remained the most common pathogen overall, non-IDU-IE cases were found to be attributed to a much broader group of pathogens including multiple different gram-negative pathogens. IDU-IE cases were additionally noted to have longer durations of bacteremia, with a mean of 4 days to blood culture clearance and multiple patients exceeding 7 days of bacteremia (longest duration, 16 days).
Effect of Inclusion of IDU-IE Cases Identified Using Nonspecific ICD-10 Code Combinations on Prospectively Identified Cases on Research Outcomes
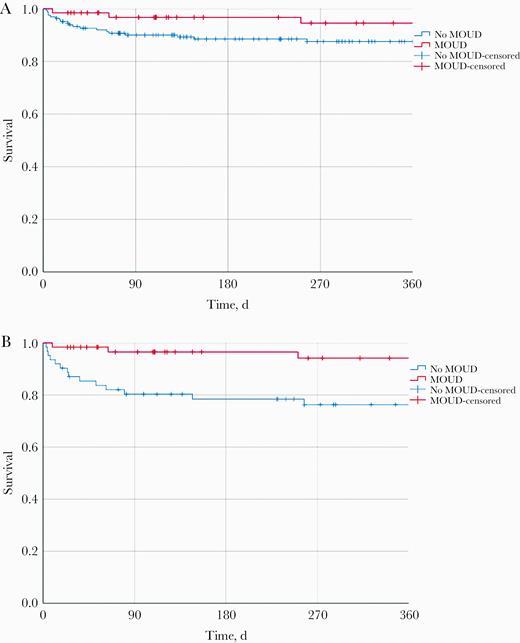
We observed substantial differences in clinical outcomes for AMA discharge and all-cause mortality between the 2 cohorts (Table 2). Specifically, when the entire cohort of 229 patients (including all prospectively identified patients and patients with an ICD-10 code combination in Supplementary Table 1 previously used to study patients with IDU-IE) was analyzed, receipt of MOUD was paradoxically associated with a trend toward an increased risk of AMA discharge (RR, 1.12; 95% CI, 0.48-2.64). In contrast, if only confirmed IDU-IE cases were analyzed, receipt of MOUD was associated with a trend toward a reduction in AMA discharges, as 6 of 62 (9.7%) patients left AMA in the MOUD group compared with 12 of 61 (19.7%) patients who did not receive MOUD (RR, 0.49; 95% CI, 0.19-1.22). Neither of these results was statistically significant; however, the apparent reversal in trend is striking. To investigate the impact inclusion of noncases would have on mortality, we performed a Kaplan-Meier analysis of survival stratified by receipt of MOUD. Patients who received either methadone or buprenorphine during their hospitalization had lower mortality rates than those who did not; however, the effect was not statistically significant when both IDU-IE cases and noncases were included in the overall population (P = .173). The effect of MOUD is magnified and becomes significant (P = .007) when only IDU-IE patients are analyzed (Figure 1).
DISCUSSION
Our results demonstrate that the ICD-10 diagnosis code combinations currently used to identify IDU-IE admissions in the administrative data research literature are not specific. Such ICD code combinations included non-IDU-IE cases with substantially different ages, comorbidities, lengths of stay, and microbiologic illnesses. Misclassification of IDU-IE cases in clinically relevant analyses biases analyses toward the null. IDU-IE-specific ICD-10 diagnosis codes are needed. Without such codes, analyses using administrative data to analyze the outcomes and epidemiology of IDU-IE should require physician review, have additional external validation, or be interpreted with caution.
Use of ICD code algorithms to identify cases of IDU-IE is becoming increasingly common as the opioid crisis continues. Large data sets, such as administrative data, have offered researchers the hope of identifying clinical practices that impact readmission rates and mortality, or identifying concerning pathogen trends early. However, our analysis raises concern that these data sets could contain non-IDU-IE cases, and actually consist of high volumes of patients with chronic pain or cancer-related pain, who have endocarditis not related to injection drug use. Inclusion of such patients could bias multiple important hypotheses toward the null. Our study demonstrates that inclusion of non-IDU-IE cases (such as patients with chronic pain and endocarditis from other causes) obscures the benefit provided by MOUD on both AMA discharge and all-cause mortality. It is easy to imagine that the inclusion of non-IDU-IE cases would dramatically alter the results of existing research, ranging from missed opportunities for provision of naloxone kits to the impact of interventions such as cardiac surgery and the cost of hospitalizations for IDU-IE.
Microbiologic outcomes were also affected. Inclusion of non-IDU-IE cases altered important epidemiologic information such as the rate of prolonged bacteremia, incidence of MSSA, and prevalence of viral hepatitis. These findings are consistent with work by other teams that has shown significant differences in causative pathogens between IDU-IE vs non-IDU-IE cases [15]. This has important impacts on economic analyses and anticipated survival analyses for IDU-IE. Furthermore, public health analyses evaluating hepatitis screening and treatment for IDU-IE will likely be biased toward underscreening and undertreating IDU-IE patients.
Systematized Nomenclature of Medicine Clinical Terms (SNOMED CT) is a comprehensive and precise international clinical reference terminology frequently used in electronic health records for clinical documentation of problem lists. Clinicians should also be aware that several SNOMED CT codes may map to a single ICD-10 diagnosis code. For example, although “heroin addiction” and “opioid dependence with daily use” are clinically distinct conditions, both of these problem list items (also known as clinician display names) map to the same ICD-10 F11.xx diagnosis code (Table 3). This underlying issue illustrates the limited utility of ICD-10 billing and claims data in administrative data research targeting IDU-IE.
Prior work in other settings has demonstrated a similar lack of sensitivity when using ICD-10 diagnosis codes to identify IDU-IE [16]. To compensate, some researchers have suggested restricting age ranges [17, 18] or adding codes for blood-borne pathogens such as hepatitis C or HIV [18]. However, this selects for PWID who preferentially engage in needle-sharing and who may have different characteristics than those using syringe exchange facilities or taking other precautions. Similarly, some studies have attempted to remove any codes related to potential substance use disorders or evaluate the intersection of hepatitis C and infective endocarditis as a proxy for IDU-IE [7]. The results from our study underscore the limitations of this strategy; while confirmed IDU-IE cases in our cohort were more likely to have a positive hepatitis C antibody (76%), a sizeable percentage (32%) of non-IDU-IE cases had a positive hepatitis C antibody (P < .001).
Importantly, this study represents the first work to compare ICD-10 code algorithms to prospective identification of IDU-IE cases in a US health care setting. That ICD code algorithms not only incorrectly identify non-IDU-IE patients but also fail to identify patients who do have IDU-IE is of significant concern. Researchers using ICD code algorithms for this purpose should attempt to adjust for misclassification, if results are intended to inform clinical practice.
The limitations of this study include its single-center design and limited timespan (2017-2020). However, the limitations related to nonspecific ICD codes would be present in all geographic regions. This study further focuses entirely on IDU-IE secondary to opioid use and does not evaluate IDU-IE secondary to injection of other substances, including methamphetamines. As use of methamphetamines continues to increase nationwide, particularly in rural areas of the country, current and future analyses will likely underestimate the true prevalence of IDU-IE secondary to methamphetamines and other nonopioids. Although our data suggest that MOUD reduce overall mortality, these analyses are complex, and our current models do not take into account patients switching between treatment groups during subsequent admissions. Thus, these results should be interpreted with caution.
The United States faces an ongoing syndemic of substance use disorders and life-threatening infectious complications associated with IDU, including infective endocarditis. It is critical that in the midst of this epidemic we have the ability to accurately measure epidemiologic trends of this syndemic. While our work only evaluates 1 specific algorithm to identify IDU-IE secondary to opioids, the lack of sensitivity is troubling. Our findings demonstrate that the current state of combining multiple nonspecific ICD-10 codes fails to consistently identify this unique cohort and likely underestimates the benefit of evidence-based treatments, such as MOUDs. We believe that the best way to overcome these significant problems is to issue a new ICD-10 code that is specific to injection drug use-associated infective endocarditis.
Supplementary Data
Supplementary materials are available at Open Forum Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Acknowledgments
Financial support. This work was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under grant numbers KL2TR002346 and T32AI007172.
Disclaimer. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Potential conflicts of interest. All authors: no conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
Patient consent. This study was granted a waiver of consent and approved by Washington University Institutional Review Board (IRB#201804183 and IRB#201907187).
References
Nguồn: https://blogtinhoc.edu.vn
Danh mục: Info
This post was last modified on Tháng mười một 29, 2024 4:33 chiều