Abstract
Introduction
Candida albicans is a common commensal organism of human skin and mucosal surfaces such as cornea, respiratory tract, oral cavity, bone marrow, intestines, bladder, and genital tract. However, it has emerged as a clinically important fungal pathogen that causes both mucosal and deep tissue infections (Pappas et al., 2004) associated with a crude mortality rate of 62%(Gudlaugsson et al., 2003). Azoles are one of several major options for invasive candidiasis, and fluconazole is used most commonly in azoles. However, long-term therapy with fluconazole facilitates the emergence of fluconazole resistance (Rex et al., 1995). In addition, C. albicans commonly exist in biofilms and easily attach on both mucosal and plastic surfaces of indwelling devices (Hasan et al., 2009). The biofilms are microbial communities that are distinct from their planktonic counterparts, and cells in biofilms bind tightly each other and display specific phenotypes (Ramage et al., 2005). As the result, the resistance of biofilms to antifungal agent is increased compared with that of planktonic cells (Kuhn & Ghannoum, 2004).
Many approaches have been used to improve the effect of antimicrobial therapy for resistant isolates, and one of them is drug combination(Khan et al., 2012). Synergism was observed when antifungal agents were combined with some nonantifungals, such as tacrolimus, cyclosporin A, and amiodarone (Guo et al., 2008; Li et al., 2008; Sun et al., 2008). In addition, Fiori et al. demonstrated that doxycycline was synergistic with fluconazole against planktonic C. albicans at a concentration of 25 mg L−1 (Fiori & Van Dijck, 2012). Other reports showed that high dose of doxycycline (≥ 128 mg L−1) in combination with traditional antifungal agents may be useful for the treatment of C. albicans biofilm infection (Miceli et al., 2009), and synergistic effect was observed on biofilms of non-albicans Candida spp. with the concentration of 512 mg L−1 of doxycycline (El-Azizi, 2007). However, the effect of lower concentration of doxycycline in combination with fluconazole against biofilms of C. albicans needs to be investigated, and so does the distinction among the combined effects on C. albicans with different susceptibilities to fluconazole.
Bạn đang xem: Synergistic effect of doxycycline and fluconazole against Candida albicans biofilms and the impact of calcium channel blockers
Calcium homeostasis is an important factor during normal growth of C. albicans and is associated with multiple aspects of fungal physiology, including morphogenesis, antifungal drug susceptibility, and virulence (Uppuluri et al., 2008). The chelation of extracellular calcium or deletion of the calcium transporters that modulate cytosolic calcium could severely reduce expression of some calcium transport proteins (Mid1, Cch1, or Pmr1), which influence the normal functions of C. albicans (Brand et al., 2009). Most of the combined antifungal activities are mediated by calcium regulation. Gupta et al. (2003) proved that antifungal activity of amiodarone is mediated by disruption of calcium homeostasis in C. albicans. In a preliminary study, we found that the combination of minocycline and fluconazole had synergistic effects on the biofilms of C. albicans, and benidipine (calcium channel blocker, antihypertensive, and anti-anginal drug used in a clinic) could significantly enhance this synergistic effect (Shi et al., 2010). However, little is known about the effect of the calcium channel blocker combined with doxycycline and fluconazole.
In this study, we investigated the in vitro combined antifungal activity of doxycycline (1-64 mg L−1) and fluconazole against biofilms of C. albicans with different susceptibilities (azole susceptible, azole-susceptible dose dependent, and azole resistant) by a microdilution checkerboard method, and such drug combination against planktonic C. albicans was also performed as a contrast to the result of biofilms. In addition, we evaluated the impact of calcium channel blocker (benidipine and nifedipine) on the drug combination of fluconazole and doxycycline against the planktonic cells and biofilms of C. albicans by plate streaking and liquid quantitative methods in order to find the clue for the further research on the synergistic mechanisms.
Materials and methods
Candida albicans isolates and medium
Ten C. albicans strains isolated from different clinical specimens with invasive fungus infection were tested in this study. They were identified according to standardized mycological methods (Pfaller et al., 2010). The susceptibilities of tested isolates to fluconazole were determined by broth dilution test according to the CLSI M27-A3 standard (Clinical. aLSI, 2008), and the break points are described as follows: minimum inhibitory concentration (MIC) ≤ 8 mg L−1 (susceptible),MIC ≥ 64 mg L−1 (resistant), 16 and 32 mg L−1 (susceptible dose dependent)(Pfaller et al., 2008a). The strains were azole susceptible (CA1, CA5, CA12, CA14, CA15, CA135), azole-susceptible dose dependent (CA137), and azole resistant (CA10, CA16, CA129), and they were maintained at −70 °C. The C. albicans (ATCC 10231) were used as quality control strains.
The isolates were propagated on yeast-peptone-dextrose (YPD) medium (1% yeast extract, 2% peptone, 2% dextrose, 2% agar; Ding Guo Biological Co. Ltd., China) at 35 °C and subcultured at least twice before experiments to ensure purity and viability. The cells were washed and diluted in sterilized phosphate-buffered saline (PBS; pH 7.2-7.4; Solarbio Science & Technology Co. Ltd., China). The liquid medium used for susceptibility testing was RPMI 1640 (GIBCO BRL, Life Technologies, Woerden, the Netherlands) with the pH adjusted to 7.0. The medium was supplemented with dextrose to a final concentration of 2% and 0.165 M morpholinepropanesulfonic acid (MOPS; Ding Guo Biological Co. Ltd.) (Diekema et al., 2009).
Drugs
The powders of fluconazole, doxycycline, and calcium channel blocker (benidipine and nifedipine) were used in this study. Fluconazole was provided by Cheng Chuang Pharmaceutical Co. Ltd., China; doxycycline and calcium channel blocker were purchased from the An Bei Ka Pharmaceutical Co. Ltd., China. Fluconazole was dissolved at a 2.56 g L−1 stock solution with distilled water. Doxycycline was prepared at a 6.4 g L−1 stock solution with dimethyl sulfoxide. Benidipine and nifedipine were dissolved at 2.56 g L−1 stock solutions with dimethyl sulfoxide, respectively, and the content of dimethyl sulfoxide in each assay was kept below 0.5%. These stock solutions were kept in storage at −70 °C until use.
Determination of MICs of planktonic cells
The interaction between doxycycline and fluconazole against ten C. albicans strains was tested according to methods of the CLSI M27-A3 (Clinical. aLSI, 2008) by a microdilution checkerboard technique in 96-well plates. The concentration of yeast suspension was standardized to 1 × 103 cells mL−1 in each well of plates with RPMI 1640 medium. The final concentration of fluconazole ranged from 1 to 512 mg L−1 for R and S-DD isolates (CA10, CA16, CA129, and CA137) and from 0.03125 to 16 mg L−1 for S isolates (CA1, CA5, CA12, CA14, CA15, and CA135). The final concentration of doxycycline ranged from 0.5 to 32 mg L−1 for all strains. The control wells were filled with yeast suspension and RPMI 1640 without antifungal agents. The 96-well plates were incubated at 35 °C for 48 h. A colorimetric reduction assay was carried out with 2, 3-bis(2-methoxy-4-nitro-5-sulfophenyl)-5-[(phenylamino)carbonyl]-2H-tet razolium hydroxide (XTT; Sigma) (Melo et al., 2007). The values of optical density (OD) were measured at 490 nm with a microtiter plate reader (Thermolabsystems Multiskan MK3). The MIC endpoint was defined as the lowest drug concentration that caused an 80% inhibition compared with that of drug-free growth control (Pfaller et al.,2008b). Each testing was carried out in duplicate and repeated three times on different days. The MIC of control strain ATCC 10231 was within the prescript of CLSI.
Determination of sessile minimum inhibitory concentrations (SMICs) of biofilms
Xem thêm : Potasio
Biofilms were formed as described by Ramage et al. (2001) on 96-well plates in modified cell suspensions being 1 × 103 cells mL−1, and we demonstrated that biofilm could form with this cellular density over at least 4-h cultivation. The biofilms were formed over four time intervals (4, 8, 12, and 24 h) at 37 °C by pipetting 100 μL of the standardized cell suspension into selected wells of 96-well plate. At each time point, the biofilms were washed three times gently with sterile PBS to remove the planktonic yeast. Fluconazole and doxycycline were then added to the biofilms in serially double-diluted concentrations. The final concentration of fluconazole in wells ranged from 1 to 512 mg L−1 for resistant isolates (CA10, CA16, CA129), from 0.5 to 256 mg L−1 for susceptible dose-dependent isolates (CA137), and from 0.25 to 128 mg L−1 for susceptible isolates (CA14, CA135, CA1, CA5, CA15, CA12). The final concentration of doxycycline in wells ranged from 1 to 64 mg L−1 for all strains. The control wells were filled with RPMI 1640 without antifungal agents. Then the whole system was incubated for a further 48 h at 35 °C. A colorimetric reduction assay was carried out with XTT according to the protocol of Melo et al. (2007). The absorbance was measured with a microtiter plate reader (Thermolabsystems Multiskan MK3) at 490 nm. The drug concentration that brought about a reduction in absorption by 80% contrasted to control well was reported as the SMIC endpoint. Each testing was carried out in duplicate and repeated three times on different days.
Drug interaction interpretation
In this study, the drug combination interaction was interpreted according to two models based on Loewe additivity (LA) and Bliss independence (BI) theories, respectively (Prichard & Shipman, 1990; Polak, 1999; Sun et al., 2009), including the fractional inhibitory concentration index (FICI) and the percentage of growth difference (△E). In FICI model, the difference between effective concentration of drugs alone and in combination was compared. In △E model, the difference between estimated combined effects based on the effects of the individual drugs and those obtained from the experiment was compared.
FICI model
The nonparametric model FICI was defined as follows: FICI = FICA + FICB = CA/MICA + CB/MICB, where MICA and MICB are the MICs of the drugs A and B used alone, and CA and CB are the MICs of the drugs A and B used in combination. The interpretation of the FICI was as Odds (Odds, 2003) suggested that: the value of FICI ≤ 0.5 revealed synergy, 0.5 < FICI ≤ 4 revealed no interaction, and FICI > 4 represented antagonism.
ΔE model
The nonparametric model ΔE was based on the BI theory, where E is the percentage of growth. Ei = EA × EB, where Ei is the predicted percentage of growth of the combination of drugs A and B, and EA and EB are growth percentage of drugs A and B used alone. Interaction between two drugs is described by the difference (ΔE) between the predicted and measured percentages of growth at various combinations. In the nonparametric approach described by Prichard et al. (1991, 1993), EA and EB are obtained directly from experimental data. When the average value of ΔE was positive and the 95% confidence interval (CI) among the three replicates did not include 0, SS (statistically significant) synergy was claimed; when the average value of ΔE was negative and the 95% CI did not include 0, SS antagonism was claimed.
To summarize the interaction between two drugs, the sums of the percentages of all SS synergistic (SSYN) and SS antagonistic (SANT) interactions were calculated. Statistically values of < 100% meant a considered weak interaction, those of 100-200% meant a considered moderate interaction, and those of > 200% meant a considered strong interaction (Meletiadis et al., 2003).
The impact of calcium channel blocker on drug combination
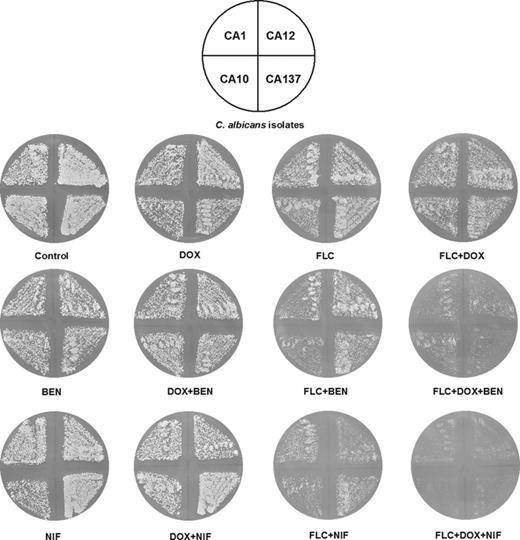
The impact of calcium channel blocker (benidipine and nifedipine) on drug combination was investigated by plate-streaking method firstly. The strains used in this experiment were CA1, CA12, CA137, and CA10. The concentration of yeast suspension was standardized to 1 × 105 cells mL−1 with PBS. Melting YPD agar was put into the culture plates with the volume of 20 mL. Drugs were added into the medium, and the final concentration was 2 mg L−1 for fluconazole, 32 mg L−1 for doxycycline, 16 mg L−1 for benidipine, and 8 mg L−1 for nifedipine. The yeast suspension was spread onto the solidified medium. At last, the plates were incubated at 35 °C for 24 h.
In order to explore the impact of calcium channel blocker on the drug combination of fluconazole and doxycycline and determine how this impact varies as the concentration of calcium channel blocker changes, a quantitative analysis in 96-well plates was performed. Planktonic cells and biofilms were prepared in the 96-well plates as described above. A given concentration of fluconazole and doxycycline was chosen in order to distinguish the difference in the impact of calcium channel blocker with various concentrations. The solution of benidipine and nifedipine was diluted with RPMI 1640 to the concentrations of 1, 2, and 4 mg L−1 and 4, 6, and 8 mg L−1, respectively. And 1 mg L−1 for benidipine and 4 mg L−1 for nifedipine are minimum effective concentrations as a result of our preliminary experiments. The 96-well plates were incubated for 48 h at 35 °C. Activities of cells in planktonic cells and biofilms were assessed by XTT assay (Melo et al., 2007). OD value was measured by a microtiter plate reader (Thermolabsystems Multiskan MK3) at 490 nm. Each testing was carried out in duplicate and repeated three times on different days. Statistical significance of the results was determined by one-way analysis of variance (anova) followed by Dunnett’s test.
Results
MICs of fluconazole in combination with doxycycline
The results of the tested drugs alone and in combination against planktonic C. albicans were summarized in Table 1. It showed that doxycycline had little effects on all strains when it was used alone; however, a potent antifungal effect was observed when in combination with fluconazole. The effects varied against strains with different susceptibilities to fluconazole. For resistant strains, an obvious synergism was observed. The MIC of fluconazole was reduced nine and seven dilutions for CA16 and CA10 with 8 mg L−1 of doxycycline, respectively, and the MICs of fluconazole were reduced six dilutions for CA129 in the presence of 2 mg L−1 of doxycycline. For susceptible dose-dependent strains (CA137), the MIC was reduced four dilutions in the presence of 1 mg L−1 of doxycycline. However, for susceptible strains, little synergism was observed, and antagonism was observed in a few wells. The differences in the MICs reduction against different isolates suggested that the synergism mediated by doxycycline was related to the susceptibilities of C. albicans. The growth percentage of each drug combination was calculated by OD values of the drug-containing wells compared with those of the drug-free control wells. Synergism was consistently interpreted by FICI and ΔE models for three resistant isolates and one susceptible dose-dependent isolate. However, different interpretations were found by these two models in six susceptible isolates.
SMICs of fluconazole in combination with doxycycline
Ten isolates with different susceptibilities to fluconazole were studied in this experiment. A consistent synergistic effect of fluconazole and doxycycline was interpreted by FICI and ΔE models against C. albicans biofilms formed over 4, 8, and 12 h. However, as the biofilms matured and its complexity increased, the synergism weakened and was scarcely observed on the biofilms that formed over 24 h (not shown). For each strain, the different combined antifungal effect appeared and was shown in Table 2.
The impact of calcium channel blocker on drug combination
Xem thêm : Can you Ovulate Without Having a Period?
The impact of calcium channel blocker (benidipine and nifedipine) on drug combination of doxycycline and fluconazole was evaluated by plate-streaking method, and the results against four isolates were shown in Fig. 1. The fungi in control group grew well as expected. Little effect was observed in single-agent group including doxycycline, benidipine, and nifedipine, and a similar result was obtained when doxycycline was combined with benidipine and nifedipine. In order to evaluate the effect of the combined drugs, low concentration of fluconazole was used in the plate-streaking test, so no obvious effect was observed when fluconazole was used alone against isolates with different susceptibilities. The addition of doxycycline or calcium channel blocker (benidipine and nifedipine) with fluconazole inhibited the fungal growth compared with fluconazole used alone, and the impact of calcium channel blocker (especially nifedipine) seemed stronger than doxycycline. Furthermore, we were surprised to find that addition of calcium channel blocker to drug combination of doxycycline and fluconazole enhanced the effect dramatically, the growth of the fungi was almost inhibited completely by the three drug combination of fluconazole, doxycycline, and nifedipine, and the effect was observed on both fluconazole-resistant and fluconazole-susceptible strains.
To explore the impact of different concentrations of calcium channel blocker on the drug combination of fluconazole and doxycycline, a liquid analysis was carried out quantitatively. Planktonic cells and biofilms of four strains (CA10, CA16, CA129, and CA137) were studied in this test. As shown in Fig. 2, a reduction in growth percentage was displayed when benidipine was added to drug combination of doxycycline and fluconazole, and progressive reductions were achieved with benidipine concentration increased. In planktonic cells (a), the effect of benidipine on the resistant strain of CA10 and CA16 is more apparent than that on CA129 and CA137, while in biofilms (b), no significant differences among four isolates were found. Compared with biofilms, sharper reductions in the growth percentage in planktonic cells appeared after the addition of benidipine. As shown in Fig. 3, decrease in growth percentages was caused by addition of nifedipine to drug combination of fluconazole and doxycycline, and the higher the concentration of nifedipine added, the better the effect achieved. In planktonic cells (a), the growth percentage reduction in CA16 was less than that in CA10, CA129, and CA137, while in biofilms (b), the effect of nifedipine on CA10 and CA16 was more apparent than that on CA129 and CA137. For the two calcium channel blockers, the antifungal activity was similar against the biofilms formed over different time intervals.
Discussion
The marked increase in the emergence of fluconazole-resistant C. albicans isolates is on account of various reasons including decreased permeability of membranes, interference with target enzyme lanosterol 14a-demethylase, decreased accumulation of antifungal agents by enhanced efflux systems, qualitative or quantitative change in ergosterol, and biofilm formation. Doxycycline is a tetracycline derivative, which is considered to be an antibacterial agent; however, it was found to act synergistically with antifungal agents against C. albicans. Oliver et al. (2008) showed that tetracycline can alter antifungal drug susceptibility of amphotericin B and terbinafine in C. albicans and other pathogenic fungi. Miceli et al. (2009) demonstrated that combination of high-dose doxycycline and azoles showed synergism against biofilms of C. albicans and non-albicans Candida spp., and a recent study showed that addition of relatively low concentration of doxycycline has a impact on prevention of fluconazole tolerance against planktonic C. albicans (Fiori & Van Dijck, 2012). Here we characterize the antifungal activity of fluconazole in combination with a given concentration of doxycycline (1-64 mg L−1) against C. albicans biofilms, and in contrast, the drug combination against planktonic C. albicans was also performed. The results of microdilution checkerboard method showed that fluconazole and doxycycline had strong synergism against planktonic cells in fluconazole-resistant isolates. However, almost no synergy was observed in fluconazole-susceptible isolates, and discrepancy in interpretations made by FICI and △E models appeared perhaps because of the different theories that they depended on. Nevertheless, both FICI and △E are still useful approaches for analyzing the interactions between different drugs in spite of some disagreement. As for biofilms, significant synergistic effect of fluconazole in combination with doxycycline has emerged against almost all C. albicans biofilms that formed over three time intervals (4, 8, and 12 h). In addition, a weaker combined antifungal effect of fluconazole and doxycycline against C. albicans biofilms was observed compared with planktonic cells, and the combined efficacy decreased with the prolonged time of biofilm formation. At the same time, we found that SMICs of fluconazole alone increased compared with MICs in almost all isolates.
Calcium is an important second messenger in developmental and stress signaling pathways of C. albicans (Yang et al., 2011). Uppuluri et al. (2008) documented that combinations of calcineurin inhibitor (tacrolimus and cyclosporin A) and fluconazole could prevent or eradicate biofilm-associated cells in C. albicans. Gamarra et al. (2010) suggested that the drug synergism of amiodarone and fluconazole is likely mediated by Ca2+ stress, and they pointed out that amiodarone causes the hyperexpression of vacuole Ca2+ pumps and calcineurin pathway genes. Benidipine is a non-selective calcium channel blocker that blocks Ca2+ channels including L- and T-type (Abe et al., 2011), and it is used commonly as antihypertensive and anti-anginal drug in clinical therapy. The preliminary study in our laboratory has found that the calcium channel blocker including benidipine altered the antifungal effect of fluconazole in combination with minocycline (Shi et al., 2010). In order to evaluate the potent relationship between calcium channel blocker and synergistic effect mediated by fluconazole and doxycycline, benidipine and nifedipine (a selective L-type calcium channel blocker) (Rouet et al., 2012) were added to drug combination in this study. In a plate-streaking method, a surprising result was discovered that a sharp inhibition of fungal growth appeared when calcium channel blocker was added into drug combination of fluconazole and doxycycline, and the effect of nifedipine is better than that of benidipine. In contrast, obvious weakening of fungal growth was observed when nifedipine was combined with fluconazole, and this antifungal activity was more obvious than that brought about by combination of fluconazole and doxycycline. In order to determine the exact impact of calcium channel blocker, a liquid method was undertaken quantitatively using planktonic cells and biofilms of the four C. albicans isolates. Enhancement of antifungal activity was observed by addition of benidipine and nifedipine to drug combination of fluconazole and doxycycline, and sharper reduction in fungal growth percentage was presented with the higher concentration of calcium channel blocker. In planktonic cells, better effects of benidipine were achieved against the isolates with stronger resistance to fluconazole, while no obvious regularity was found with nifedipine. In biofilms, the effects of benidipine on all four isolates were similar, while the effect of nifedipine is more obvious on the isolates with stronger resistance to fluconazole (Figs 2 and 3). These findings disclosed that the doxycycline-mediated synergism can be enhanced by benidipine and nifedipine, which suggested that the blocking of calcium channel can promote the combined effect of fluconazole and doxycycline. Fiori and collaborators reported that doxycycline-mediated growth inhibition can be reversed by externally added iron, which indicates that iron depletion may account for the synergism (Fiori & Van Dijck, 2012). In this study, it is possible that calcium homeostasis may account for the synergism since calcium is another indispensable ion in C. albicans. However, further study is needed to investigate the relationship of various effects caused by different calcium channel blockers and the potential mechanisms involved in the expression of some proteins and genes, such as Ca2+ transporters of Cbicans, including pumps (Pmr1 and Pmc1), channels (Cch1, Mid1, and Yvc1), exchangers(Vcx1), and transcription factor (RIM101) involved in the cation overload response (Cui et al., 2009).
Candida albicans biofilms are complex microbial communities consisting of yeast, hyphae, and pseudohyphae (Sudbery et al., 2004). The structure of biofilms maintains stable, and they are highly resistant against most commonly used antimycotics. Ramage et al. (2002) demonstrated that C. albicans biofilm resistance is multifactorial and cannot be explained by one mechanism alone, and expression of genes encoding efflux pump including CDR1, CDR2, and MDR1 was upregulated during the formation and development of C. albicans biofilms. Our study showed that in the presence of doxycycline and fluconazole, a great growth inhibition against resistant C. albicans and C. albicans biofilms appeared. The relationship between this synergistic effect and resistance mechanism including efflux pump genes needs further study.
In conclusion, this study suggested that the antifungal effect of fluconazole could be sensitized by doxycycline against C. albicans biofilms and resistant C. albicans, and the synergism of this combination can be enhanced by calcium channel blocker. This result is of great significance in looking for new antifungal agents and provides a reliable basis to further exploration of calcium-mediated antifungal mechanism. The mechanisms including the expression of Ca2+ transporters and efflux pump genes in C. albicans are under research in our laboratory now.
Authors’ contributions
Y.G. and C.Z. contributed equally to this work.
Conflict of interest
We declare that we have no conflict of interest.
Acknowledgements
We are grateful to Department of Science and Technology of Shandong Province (2007GG20002026 and ZR2011HL049) for the financial support, and we thank Central Laboratory for technical assistance as well as Clinical Microbiology Room of Qianfoshan hospital for providing the isolates used in this study.
References
Author notes
Nguồn: https://blogtinhoc.edu.vn
Danh mục: Info
This post was last modified on Tháng mười một 23, 2024 4:08 chiều