Introduction
Acute myocardial infarction (AMI) is a serious medical condition characterized by myocardial injury or death due to a sudden reduction in blood supply to the heart. Despite significant advances in AMI prognosis in the last decade, it remains a leading cause of morbidity and mortality worldwide.1-3 AMI is traditionally classified into two types: ST-elevation myocardial infarction (STEMI) and non-ST-elevation myocardial infarction (NSTEMI), based on the manifestation observed on the electrocardiogram (ECG). Although STEMI and NSTEMI share similar risk factors and etiology, they differ in terms of pathophysiology, epidemiology, and severity.1-4 Therefore, the European Society of Cardiology (ESC) and the American Heart Association (AHA) regularly update guidelines for the management of STEMI and NSTEMI separately.5-10
In most cases, AMI is caused by a ruptured atherosclerotic plaque or erosion of the coronary artery endothelium, triggered by inflammation and followed by thrombosis. STEMI occurs when the thrombosis completely blocks the coronary artery, while NSTEMI occurs when the thrombus is not fully occlusive.1,3 STEMI accounts for approximately 25-40% of all AMIs and is associated with higher short-term mortality rates, while NSTEMI is more common in older patients with a higher prevalence of comorbidities.1,3,4 The management of STEMI involves urgent reperfusion therapy with primary percutaneous coronary intervention (PCI) within a few hours of symptom onset. On the other hand, NSTEMI is managed with antiplatelet, anticoagulant, and statin therapies, and urgent PCI is reserved for high-risk cases.3,4,8,10
Administrative claims data refers to electronic health data collected and maintained by health insurers and public programs for administrative purposes. It typically includes patient demographics, diagnoses, procedures, prescriptions, and other longitudinal healthcare-related information. For example, Taiwan’s National Health Insurance (NHI) claims database is one of the world’s largest comprehensive administrative claims databases.11-13 Administrative claims data has been widely used in cardiovascular research. However, there are limitations to its use, such as potential inaccuracies in diagnosis coding, which can impact the reliability of research findings. Therefore, it is essential to validate claims data by comparing it with primary medical data and definitive diagnoses to ensure the quality and reliability of the data used in research.
In 2014, Cheng et al conducted a study to evaluate the accuracy of the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnostic code (410) for identifying patients with AMI in Taiwan’s NHI claims data.14 They found a sensitivity of 0.88 and a positive predictive value (PPV) of 0.92 for identifying AMI patients with a first diagnostic code of 410. However, the accuracy of individual ICD diagnostic codes for STEMI and NSTEMI in the claims data has not been verified. Additionally, since 2016, Taiwan’s NHI claims database has switched to using the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) diagnostic codes, which provide more specific classification for STEMI and NSTEMI. Given the distinct epidemiological profiles, pathophysiology, severity, and management approaches of STEMI and NSTEMI, it is crucial to separately examine these two types of AMI when utilizing nationwide real-world claims data. However, there is a lack of research validating the accuracy of ICD-10-CM codes in identifying STEMI and NSTEMI patients in Taiwan’s NHI claims database. To address this gap, the current study aims to develop and validate case definition algorithms separately for STEMI and NSTEMI based on ICD-10-CM codes in Taiwan’s NHI claims database, using data from two hospitals in Taiwan.
Materials and Methods
Study Settings
This retrospective study was conducted at two hospitals in Taiwan that have a contractual agreement with Taiwan’s NHI program. The NHI program covers almost all hospitals in Taiwan and requires NHI-contracted hospitals to submit claims in a standardized format to the NHI Administration. The two participating hospitals were among the 46 accredited advanced emergency-responsibility hospitals in the country that offer 24/7 emergency cardiac catheterization services.15,16
To develop case definition algorithms, we obtained a dataset from the Ditmanson Medical Foundation Chia-Yi Christian Hospital, a private tertiary teaching hospital with 1000 beds and an annual volume of approximately 500 admissions for AMI. For external validation of these algorithms, we obtained a dataset from the Buddhist Dalin Tzu Chi General Hospital, a private tertiary hospital with 800 beds and approximately 200 AMI admissions per year. We selected this hospital for external validation because it is part of a large healthcare organization that includes eight hospitals across both urban and rural areas in Taiwan that use the same electronic medical record (EMR) system and health information system.
The study protocol was reviewed and approved independently by the institutional review boards of both hospitals, with a waiver of informed consent (approval numbers: Ditmanson Medical Foundation Chia-Yi Christian Hospital IRB2022088 and Buddhist Dalin Tzu Chi General Hospital B11201017).
Taiwan’s National Health Insurance Claims Database
Taiwan’s NHI program was launched in 1995 as a compulsory single-payer healthcare system to provide affordable healthcare to all residents. It includes a wide range of services, such as inpatient care, outpatient care, laboratory testing, prescriptions, dental services, home care, and preventative services. The NHI claims database contains the longitudinal claims of nearly 99.8% of Taiwan’s population, making it a valuable resource for research on disease prevalence, healthcare policies, and long-term prognosis.11,17 The NHI claims data includes outpatient claims, inpatient claims, prescriptions dispensed at pharmacies, and registries for beneficiaries, medical facilities, and board-certified specialists. These datasets can be linked with encrypted personal identification numbers to provide patient-level information on demographic characteristics.11 The NHI claims database released for research allows a maximum of three diagnoses on outpatient claims and five diagnoses on inpatient claims. Diagnoses are coded using the ICD-9-CM until 2015 and the ICD-10-CM from 2016 onwards.
Data Sources and Participants
The case definition algorithms were developed using data obtained from the Ditmanson Research Database, a deidentified research database containing both administrative claims data and EMRs. This database includes clinical information for approximately 1.4 million patients who received healthcare at the Ditmanson Medical Foundation Chia-Yi Christian Hospital between January 2006 and December 2022, with 0.6 million inpatient and 21.5 million outpatient records. To develop case definition algorithms for STEMI and NSTEMI based on ICD-10-CM diagnostic codes, we extracted claims data and medical records for all inpatients treated between January 2016 and December 2021. For external validation of the algorithms, we used data extracted from the EMRs and claims data of all inpatients treated at the Buddhist Dalin Tzu Chi General Hospital during the same period.
Case Definition Algorithms
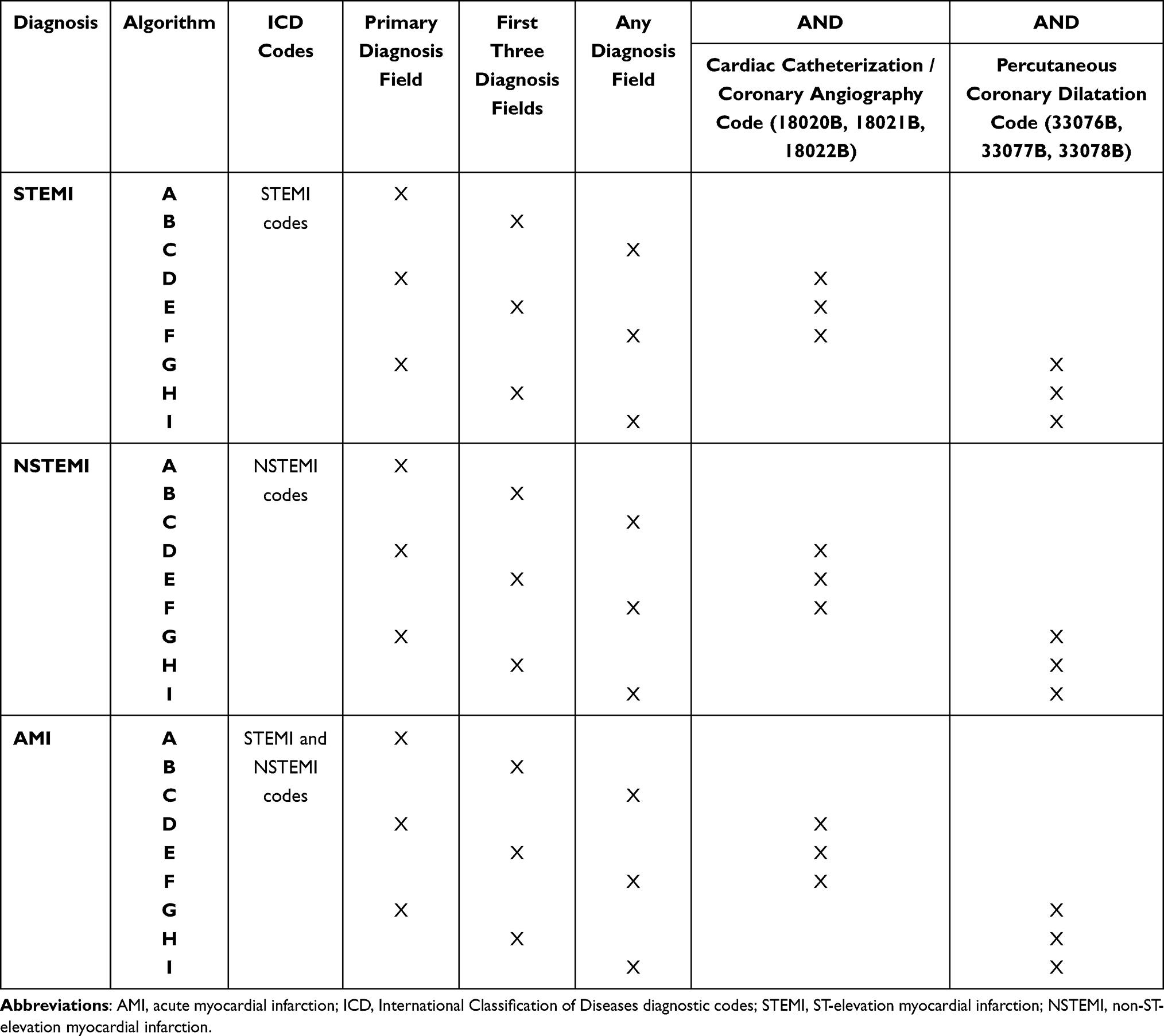
Table 1 presents the algorithms used to identify STEMI, NSTEMI and AMI from the NHI claims data. The algorithms relied on the presence of ICD diagnostic codes (Supplementary Table 1). Variations to the primary algorithm included: 1) the position of the ICD codes, such as the primary diagnosis field, the first three diagnosis fields, or any diagnosis field, 2) the presence of billing codes for cardiac catheterization or coronary angiography (18020B, 18021B or 18022B), and 3) the presence of a billing code for percutaneous coronary dilatation (33076B, 33077B or 33078B).
Table 1 Case Definition Algorithms for STEMI, NSTEMI, and AMI
Ascertainment of ST-Elevation and Non-ST-Elevation Myocardial Infarction
To identify all patients with STEMI and NSTEMI, we used three screening methods: keyword search, ICD code search, and procedure code search, as shown in Figure 1. For the keyword search, we screened the diagnoses recorded in the discharge summary of all inpatients during the study period for keywords related to AMI (Supplementary Table 2) to identify potential AMI cases. The ICD and procedure code search utilized ICD diagnostic codes related to AMI (Supplementary Table 1) and procedure codes associated with coronary angiography and interventions (Supplementary Table 3) to identify potential AMI cases from all inpatient claims during the study period.
Figure 1 Flow chart outlining the verification process of true AMI cases.
Abbreviations: AMI, acute myocardial infarction; ICD, International Classification of Diseases diagnostic codes; STEMI, ST-elevation myocardial infarction; NSTEMI, non-ST-elevation myocardial infarction.
We manually reviewed the medical records, serial troponin levels, serial ECG reports, and coronary angiography reports of the identified potential AMI cases to determine whether each patient had a true STEMI or NSTEMI, based on the newest universal definition of myocardial infarction.2,10 In brief, to diagnose AMI, several criteria were considered. First, the patient’s cardiac troponin value needed to exceed the 99th percentile upper reference limit, and this value had to change by over 20% in serial examination. Second, the patient’s medical records showed symptoms and/or signs related to clinical myocardial ischemia. Third, the ECG exhibited new ischemic or ST-segment changes. Fourth, the patient’s coronary angiography indicated the presence of a coronary thrombus or occlusion of the coronary artery. The differential diagnosis between STEMI and NSTEMI was primarily based on the ECG manifestations.2 The diagnostic criteria were shown in Supplementary Table 4. Two investigators (MJT and JHL) conducted the review, and any discrepancies were resolved by consensus or by a third investigator (JFL). The consensus diagnosis was considered the gold standard for all analyses (Figure 1).
Analysis and External Validation
We evaluated the performance of each algorithm in identifying true STEMI and NSTEMI cases by calculating sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) based on the confusion matrix (Figure 2). We also calculated their 95% confidence intervals (CIs) using the Clopper-Pearson exact method. The primary evaluation metric was the kappa coefficient, which was used to measure the agreement between algorithm-detected AMI cases and true AMI patients. We interpreted the degree of agreement as follows: “slight” (0.00-0.20), “fair” (0.21-0.40), “moderate” (0.41-0.60), “substantial” (0.61-0.80), and “perfect” (0.81-1.00).18
Figure 2 Sample validation matrix analyzing algorithm performance against the reference standard.
Abbreviations: PPV, positive predictive value; NPV, negative predictive value; STEMI, ST-elevation myocardial infarction; NSTEMI, non-ST-elevation myocardial infarction.
We externally validated the algorithms with the highest kappa coefficients on an independent dataset from the Buddhist Dalin Tzu Chi General Hospital. A similar process was undertaken to identify potential AMI cases, and one investigator (TYT) determined if each patient was a true STEMI or NSTEMI using the same criteria. Additionally, we performed subgroup analysis by stratifying the data based on the year of admission and sex to examine any variations in accuracy among different subgroups. Subgroup differences in sensitivity and PPV were assessed using a likelihood ratio test. All data analyses were conducted using Stata 17.0 (StataCorp, College Station, Texas), and we considered statistical significance to be two-tailed p <0.05.
Results
During the study period, 197,490 inpatient visits were retrieved from the hospital inpatient claims. The keyword search identified 3776 potential cases of AMI, of which 741 were adjudicated as true STEMI and 1450 as true NSTEMI through manual chart review (Figure 1). The ICD code search identified 2489 potential cases of AMI, of which 786 were adjudicated as true STEMI and 1530 as true NSTEMI through chart review. The procedure code search identified 8762 potential cases of AMI, of which 754 were adjudicated as true STEMI and 1349 as true NSTEMI. In total, 809 cases of STEMI and 1697 cases of NSTEMI were ascertained during the study period.
The validity results of the best and all algorithms for identifying STEMI, NSTEMI and AMI are presented in Table 2 and Supplementary Table 5, respectively. The best algorithm for identifying STEMI cases was algorithm B. It defined STEMI as the presence of any STEMI ICD code (ICD-10-CM codes: I21.0, I21.1, I21.2, I21.3, I21.9) in the first three diagnosis fields. Its sensitivity, specificity, PPV, NPV, and kappa were 93.6%, 100%, 89.4%, 100%, and 0.914, respectively. For identifying NSTEMI cases, algorithm C was the best. It defined NSTEMI as the presence of the NSTEMI ICD code (ICD-10-CM codes: I21.4) in any diagnosis fields. Its sensitivity, specificity, PPV, NPV, and kappa were 82.6%, 100%, 96.5%, 99.8%, and 0.889, respectively. The best algorithm for identifying AMI cases (including STEMI and NSTEMI) was algorithm C. It defined AMI as the presence of either STEMI or NSTEMI ICD codes in any diagnosis fields. Its sensitivity, specificity, PPV, NPV, and kappa were 89.4%, 99.9%, 95.6%, 99.9%, and 0.923, respectively.
Table 2 Performance of the Best Algorithms in Identifying STEMI, NSTEMI, and AMI Among All in-Patients (n = 197,490) in the Development Dataset
Incorporating billing codes for coronary angiography and interventions in the algorithms led to a minor increase in PPV and a minor decrease in sensitivity for STEMI case detection (Supplementary Table 5, STEMI algorithms E to I). However, this resulted in a marked decrease in sensitivity and kappa for detecting NSTEMI and AMI cases, despite a slight improvement in PPV (Supplementary Table 5, NSTEMI and AMI algorithms E to I).
Table 3 summarizes the reasons for false-positive and false-negative identifications of STEMI, NSTEMI, and AMI by their respective best algorithms. In STEMI algorithm B, the primary reasons for false negatives were STEMI codes being listed in the 4th or 5th diagnosis field and STEMI cases being miscoded as atherosclerotic heart disease (I25.1) or underlying diseases. False positives for algorithm B in detecting STEMI cases were mainly caused by cases of NSTEMI or unstable angina being miscoded as STEMI. Regarding NSTEMI algorithm C, the main reasons for false negatives were being miscoded as comorbidity, underlying diseases, atherosclerotic heart disease, or STEMI. False positives in NSTEMI algorithm C were caused by unstable angina cases or suspicious cases without coronary angiography confirmation being miscoded as NSTEMI. Similar reasons for false negative and false positive results in using algorithm C in detecting AMI cases were also found, as listed in Table 3.
Table 3 Reasons for False-Negative and False-Positive Identification of STEMI, NSTEMI and AMI by the Best Algorithms
The most effective algorithms for identifying STEMI, NSTEMI, and AMI were validated using an external dataset from a different hospital, which included 152,793 inpatient visits. Table 4 shows the sensitivity, specificity, PPV, NPV, and kappa values of these algorithms. The results demonstrated that these algorithms effectively identified STEMI, NSTEMI, and AMI among the external cohort.
Table 4 Performance of the Best Algorithms in Identifying STEMI, NSTEMI, and AMI Among All in-Patients (n = 152,793) in the Validation Dataset
Xem thêm : How to Make the Most of the Fleeting Fall Weather
To assess whether the coding accuracy of the best individual algorithms was affected by the year of admission or sex, we conducted subgroup analyses stratified by the year of admission (Figure 3) and sex (Table 5). The performance of the STEMI algorithm B remained consistent throughout the years, with no significant changes in sensitivity (p = 0.312) and PPV (p = 0.317) from 2016 to 2021 (Figure 3). However, significant differences in sensitivity were observed for the NSTEMI algorithm C (p = 0.011) and AMI algorithm C (p = 0.004) among the different year subgroups (Figure 3). Regarding sex subgroups, the algorithms generally performed better in male patients compared to female patients. Significant differences were found in the sensitivity of the STEMI algorithm B (p = 0.014) and AMI algorithm C (p = 0.001), as well as the PPV of the AMI algorithm C (p = 0.038) (Table 5).
Table 5 Performance of the Best Algorithms Among Different Subgroups Stratified by Sex
Figure 3 The sensitivity and PPV of the best algorithms for identifying STEMI (A), NSTEMI (B) and AMI (C) from 2016 to 2021.
Abbreviations: PPV, positive predictive value; STEMI, ST-elevation myocardial infarction; NSTEMI, non-ST-elevation myocardial infarction.
Note: *Significant difference (P < 0.05) compared to the reference year of 2016.
Discussion
In this study, we developed and evaluated case definitions for STEMI, NSTEMI, and AMI separately using ICD-10-CM codes and billing codes for coronary angiography and interventions in Taiwan’s NHI claims database. The algorithm that defined STEMI using STEMI ICD codes in the first three diagnosis fields demonstrated the best performance. For identifying NSTEMI, the algorithm utilizing the NSTEMI ICD code listed in any diagnosis field exhibited superior performance. The algorithm that included either STEMI or NSTEMI ICD codes listed in any diagnosis field demonstrated excellent performance in defining AMI. All three algorithms exhibited satisfactory performance during external validation.
Over the past two decades, there has been a significant increase in research utilizing administrative databases to investigate cardiovascular diseases. The number of publications in this field has substantially grown, from only two publications in 1996 to 268 publications in 2018.13 Furthermore, these publications have received considerable attention, as evidenced by their citation rates.13 However, before utilizing administrative databases for epidemiological and population health research, it is crucial to develop and validate case definitions.
Several studies have examined the validity of ICD codes for diagnosing AMI in various health administrative databases, including regional and national registries. For example, Kiyota et al (2004) validated the ICD-9-CM discharge diagnostic codes (410.X0 and 410.X1) for AMI in the US Medicare system. They reported a PPV of 94.1% when considering hospitalization for at least 3 days and diagnostic codes in the principal or secondary diagnostic field.19 Similarly, Kimm et al assessed the validity of ICD-10-CM codes (I21.x) in the Korean National Medical Health Insurance claims data. They found PPVs ranging from 71.4% to 73.1% based on different criteria.20 Nakai et al conducted a validation study using the Japanese Registry Of All cardiac and vascular Disease database. They demonstrated satisfactory accuracy in identifying AMI using the ICD-10-CM code (I21.x), with a sensitivity of 78.9% and a PPV of 78.8%. The PPV increased to 84.9% when emergency hospitalization was considered.21 Based on these findings, hospitalization is an important criterion for improving the accuracy of AMI diagnosis using ICD codes. Therefore, our study focused on hospitalized patients and utilized inpatient claim data to define AMI. It is essential to note that our findings for defining AMI will be limited to studies that use inpatient claim data from Taiwan’s NHI database.
A recent analysis, using bibliometric and text mining techniques on PubMed, examined the prevalent research topics based on Taiwan’s NHI claims database.12 The findings revealed that, unlike stroke, AMI is not a primary focus of research utilizing Taiwan’s NHI claims database. This disparity suggests that the limited emphasis on AMI research may be attributed to inadequate definition and validation of STEMI and NSTEMI within the database. A previous study assessed the accuracy of using ICD-9-CM diagnostic codes to identify AMI patients in Taiwan’s NHI claims data, demonstrating satisfactory validity (sensitivity: 0.88, PPV: 0.92).14 However, it is noteworthy that Taiwan’s NHI database has transitioned to the ICD-10-CM coding system since 2016, and there is currently a lack of validation research in this context. Additionally, there is a dearth of studies examining the validity of ICD codes for the individual diagnosis of STEMI and NSTEMI. Therefore, we believe that this study will provide a critical and meaningful reference for future AMI research using Taiwan’s NHI claims database.
Previous studies have shown that transitioning from one coding system to another can lead to inconsistent estimation of disease prevalence when using diagnostic codes.22,23 In 2016, the NHI in Taiwan switched from the ICD-9-CM to ICD-10-CM coding system. Our previous study indicated that this transition had an impact on the validity of identifying out-of-hospital cardiac arrest cases using ICD-10-CM-based algorithms, with an observable decrease in validity in the first year after the transition.24 This might be due to unfamiliarity with the new coding system and potential coding errors. To examine whether a similar issue existed in the development of our algorithms, we performed a subgroup analysis to assess the accuracy of the algorithm in different years. Figure 3 shows that the STEMI algorithm demonstrated consistent performance across different years. However, we observed a significantly lower sensitivity in the year 2016 compared to the years 2017, 2018, and 2020 for both our NSTEMI and AMI algorithms. This suggests that the transition to the ICD-10-CM coding system may have affected the validity of our NSTEMI and AMI algorithms. Nevertheless, the performance of the two algorithms is still acceptable However, researchers should remain cautious regarding the decrease in validity observed in the first year following the coding system transition.
Prior research has highlighted sex disparities in the characteristics, pathophysiology, presentation, management, and outcomes of STEMI and NSTEMI.3,25 To evaluate the potential impact of sex on the accuracy of our developed algorithms, we conducted another subgroup analysis (Table 5). The results revealed differences in sensitivity for the STEMI and AMI algorithms, as well as the PPV for the AMI algorithm, between males and females. Generally, the algorithms performed better in male patients compared to female patients. However, it is worth mentioning that, overall, our developed algorithms demonstrated satisfactory performance for both sexes.
In our study, we noted false-positive identification of STEMI or NSTEMI cases, primarily due to miscoding as the opposite type of AMI, unstable angina, or suspected cases without confirmation through coronary angiography. To ensure the accuracy of our study, we specifically defined AMI cases based on evidence from coronary angiography, including the presence of a thrombus or occlusion. Therefore, cases without confirmation through coronary angiography were not considered true AMI cases. Although this approach may have slightly reduced the PPV, it ensures the reliability of our results. On the other hand, false-negative identification of different types of AMI primarily occurred when cases were miscoded as comorbidities, underlying diseases, or atherosclerotic heart disease instead of the correct type of AMI. This issue was more prominent in identifying NSTEMI cases, leading to a reduction in sensitivity for detecting NSTEMI cases. However, it is important to note that NSTEMI cases differ from STEMI cases. A significant proportion of NSTEMI patients have other comorbidities or NSTEMI occurs as a secondary condition to other primary diseases.1,3,4 This complexity in NSTEMI diagnosis might account for the observed reduction in sensitivity, which is reasonable given the multifaceted nature of NSTEMI.
This study has several limitations. Firstly, the algorithms were developed using data from only one hospital, as in previous studies.14,19,26 Therefore, it is unclear whether the findings can be generalized to the entire population covered by Taiwan’s NHI. However, all hospitals in Taiwan are required to be accredited and follow the same data processing systems for reimbursement. At a minimum, the developed algorithms performed well on an external dataset from another accredited advanced emergency-responsibility hospital. This suggests that our findings are likely to be applicable to the 46 accredited advanced emergency-responsibility hospitals in Taiwan. Secondly, the algorithms for identifying STEMI, NSTEMI, and AMI can only be applied to studies using Taiwan’s NHI database. Future studies may be required to explore the applicability of these algorithms in databases from other healthcare systems with similar coding practices. To the best of our knowledge, there is a lack of research validating the accuracy of ICD-10-CM codes in identifying STEMI and NSTEMI patients separately in other national claims databases. Therefore, the methods used in this study could serve as a reference for developing algorithms in other healthcare systems for future research. Thirdly, this study only validated the individual ICD-10-CM diagnostic codes for STEMI and NSTEMI, and the findings may not apply to the ICD-9-CM code era in Taiwan’s NHI database. Fourthly, the algorithms developed in this study only included the procedure codes, such as coronary angiography and intervention. Further studies may be needed to investigate whether adding medication codes, length of hospital stay, or the condition of post-hospital discharge follow-up could improve the diagnostic performance. Lastly, the universal definition of myocardial infarction may change with advancements in medical testing. Therefore, our results may not be applicable if there are changes in the definition of AMI in the future.
Conclusion
In Taiwan, a national acute coronary syndrome registry existed in the past, but it only covered limited years (2008-2010 and 2012-2015) and did not include hospitals nationwide.27,28 Therefore, if future studies aim to investigate the impact of new drugs, interventions, or public health events such as the COVID-19 pandemic on different types of AMI, the NHI database will be a valuable resource. However, before conducting epidemiological studies using claims databases, it is essential to validate the case definitions of the disease of interest. Currently, Taiwan’s NHI claims database lacks validated case definitions for STEMI and NSTEMI as separate entities. In this study, we developed and evaluated multiple case definition algorithms for STEMI and NSTEMI using ICD-10-CM diagnostic codes and billing codes for NHI reimbursement. The results of this study will provide valuable guidance for future researchers, allowing them to use appropriate case definitions for STEMI and NSTEMI that align with their specific research objectives.
Nguồn: https://blogtinhoc.edu.vn
Danh mục: Info
This post was last modified on Tháng mười một 21, 2024 5:13 chiều